Click the topics below for actionable strategies to address this domain 🔽
Building trust is essential to the health and well-being of employees which impacts the health and well-being of an organization (1). Trust can be intentionally built into the culture and supported by the structural design of labor models in the following ways:
- Implementing strategies to:
- Creating cultures that truly support
References:
- Özgür, G., & Tektaş, P. (2018, October). An examination of the correlation between nurses’ organizational trust and burnout levels. Applied Nursing Research, 43, 93–97. https://doi.org/10.1016/j.apnr.2018.07.004
- Kelly, L. A., & Lefton, C. (2017, November 1). Effect of Meaningful Recognition on Critical Care Nurses’ Compassion Fatigue. American Journal of Critical Care, 26(6), 438–444. https://doi.org/10.4037/ajcc2017471
- Sihvola, S., Kvist, T., & Nurmeksela, A. (2022, May 2). Nurse leaders’ resilience and their role in supporting nurses’ resilience during the COVID‐19 pandemic: A scoping review. Journal of Nursing Management. https://doi.org/10.1111/jonm.13640
- Markey, K., Ventura, C. A. A., Donnell, C. O., & Doody, O. (2020, November 6). Cultivating ethical leadership in the recovery of COVID‐19. Journal of Nursing Management, 29(2), 351–355. https://doi.org/10.1111/jonm.13191
- Hofmeyer, A., & Taylor, R. (2020, October 15). Strategies and resources for nurse leaders to use to lead with empathy and prudence so they understand and address sources of anxiety among nurses practising in the era of COVID‐19. Journal of Clinical Nursing, 30(1–2), 298–305. https://doi.org/10.1111/jocn.15520
- Xu, J. M., Stark, A. T., Ying, B. H., Lian, Z. M., Huang, Y. S., & Chen, R. M. (2022, June 13). Nurses’ Workplace Social Capital and the Influence of Transformational Leadership: A Theoretical Perspective. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.855278
- Medeiros, M. (2022, June). Nurse manager succession planning for unit health and well-being. Nursing Management, 53(6), 41–43. https://doi.org/10.1097/01.numa.0000831436.38442.a8
- Morganstein, J. C., & Flynn, B. W. (2021, March 11). Enhancing Psychological Sustainment & Promoting Resilience in Healthcare Workers During COVID-19 & Beyond. Journal of Occupational &Amp; Environmental Medicine, 63(6), 482–489. https://doi.org/10.1097/jom.0000000000002184
- Irshad, M., Majeed, M., & Khattak, S. A. (2021, June 21). The Combined Effect of Safety Specific Transformational Leadership and Safety Consciousness on Psychological Well-Being of Healthcare Workers. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.688463
- Dall’Ora, C., Ball, J., Reinius, M., & Griffiths, P. (2020b, June 5). Burnout in nursing: a theoretical review. Human Resources for Health, 18(1). https://doi.org/10.1186/s12960-020-00469-9
- Kelly, L. A., Weston, M. J., & Gee, P. M. (2021, October). A Nurse Leader’s Guide to Reducing Burnout: Nurse Leader, 19(5), 467–473. https://doi.org/10.1016/j.mnl.2021.03.012
- Centers for Disease Control and Prevention (CDC). (2021, November 30). Protecting Health Worker Mental Health: A Call-to-Action Webinar . YouTube. Retrieved May 2, 2022.
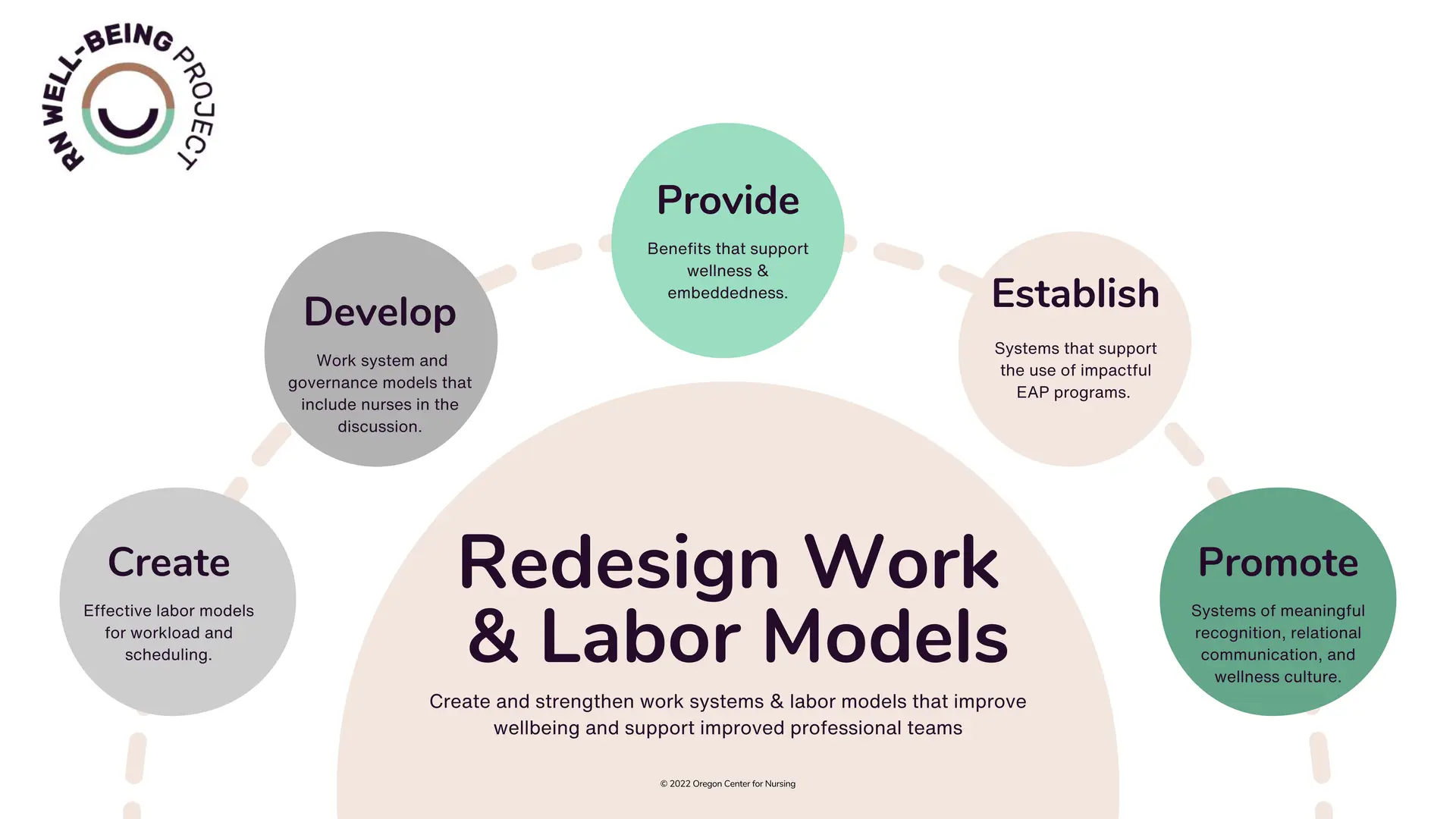
Individualized and focused initiatives to both strengthen job embeddedness and address multiple areas of well-being are important. At minimum, there are basic needs that organizations can consider: (1)
- Access to whole person supports (medical and mental health benefits, housing stability, child-care support, etc.). (1)
- Access to paid sick leave, vacation, and mental health leave with impunity. (1)
- Fair/dignified wages. (1)
- Flexibility in work schedules. (1)
- Develop a strong EAP program and reduce stigma by supporting resource use. (1,2,3)
References:
- Centers for Disease Control and Prevention (CDC). (2021, November 30). Protecting Health Worker Mental Health: A Call-to-Action Webinar . YouTube. Retrieved May 2, 2022.
- Schlak, A. E., Rosa, W. E., Rushton, C. H., Poghosyan, L., Root, M. C., & McHugh, M. D. (2022, January). An expanded institutional- and national-level blueprint to address nurse burnout and moral suffering amid the evolving pandemic. Nursing Management, 53(1), 16–27. https://doi.org/10.1097/01.numa.0000805032.15402.b3
- National Academies of Sciences, Engineering, and Medicine, National Academy of Medicine, & Well-Being, C. O. S. A. T. I. P. C. B. S. C. (2020, January 2). Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being (1st ed.). National Academies Press.
The pandemic uncovered the deep-rooted lack of wellness for nurses, which lies within systemic issues such as heavy workloads, poor collaboration, and communication that often hinder a nurse’s ability to provide quality patient care (1,2). Alterations in the development of education, labor, and management models can greatly improve wellness. Some things to consider are:
- Establish a strong academic-practice partnership to collaborate on the evolved preparedness of students so that they are ready for practice environments. (3)
- Increase engagement/structure for nurses to be involved in nursing governance within institutions. (1)
- Create/Evaluate nursing professional development paths in organizations. (4)
- Incorporate nurses in managing nurse staffing. (4)
- Promote practices that do not foster fatigue and burnout related to workload (eliminate mandatory overtime, create staffing minimums, support nurses asking for vacation, etc.). (4)
- Ensure nurse staff are taking breaks. (1,4)
- Schedule 40 hours per week or less. (1)
- Reduce time spent at home/off the clock on work-related tasks. (5)
- Manage staffing ratios. (5)
- Create flexible float pools. (6)
- Focus on the retention of nurses. (6)
- Develop creative work/schedule models that fit how nurses want to work and live. (6)
- Foster transdisciplinary training, education, and communication. (4)
References:
- Kelly, L. A., Weston, M. J., & Gee, P. M. (2021, October). A Nurse Leader’s Guide to Reducing Burnout: Nurse Leader, 19(5), 467–473. https://doi.org/10.1016/j.mnl.2021.03.012
- Dall’Ora, C., Ball, J., Reinius, M., & Griffiths, P. (2020, June 5). Burnout in nursing: a theoretical review. Human Resources for Health, 18(1). https://doi.org/10.1186/s12960-020-00469-9
- Leaver, C. A., Stanley, J. M., & Goodwin Veenema, T. (2022, February 23). Impact of the COVID-19 Pandemic on the Future of Nursing Education. Academic Medicine, 97(3S), S82–S89. https://doi.org/10.1097/acm.0000000000004528
- Schlak, A. E., Rosa, W. E., Rushton, C. H., Poghosyan, L., Root, M. C., & McHugh, M. D. (2022, January). An expanded institutional- and national-level blueprint to address nurse burnout and moral suffering amid the evolving pandemic. Nursing Management, 53(1), 16–27. https://doi.org/10.1097/01.numa.0000805032.15402.b3
- Dyrbye, L. N., Shanafelt, T. D., Sinsky, C. A., Cipriano, P. F., Bhatt, J., Ommaya, A., West, C. P., & Meyers, D. (2017, July 5). Burnout Among Health Care Professionals: A Call to Explore and Address This Underrecognized Threat to Safe, High-Quality Care. NAM Perspectives, 7(7). https://doi.org/10.31478/201707b
- UKG and Wolters Kluwer. (2022). Nursing’s Wake Up Call: Change is Now Non-Negotiable. UKG and Wolters Kluwer.
Work systems designed around relational coordination (communicating and relating for the purpose of task integration) not only increase efficiencies but have been known to improve the well-being of nurses in all practice environments. (1)
Steps that can be taken to drive positive results are:
- Improve the quality of communication and relationships among staff. (1,2)
- Create synergy and remove redundancies in shared technologies. (1)
- Establish shared goals. (1)
- Promote education and collaboration for better role understanding. (1,2)
- Integrate value and respect into the cultural norm. (1,2)
- Encourage interprofessional teamwork, collaboration, and professionalism (1,2,3)
References:
- Havens, D. S., Gittell, J. H., & Vasey, J. (2018, March). Impact of Relational Coordination on Nurse Job Satisfaction, Work Engagement and Burnout. JONA: The Journal of Nursing Administration, 48(3), 132–140. https://doi.org/10.1097/nna.0000000000000587
- National Academies of Sciences, Engineering, and Medicine, National Academy of Medicine, & Well-Being, C. O. S. A. T. I. P. C. B. S. C. (2020, January 2). Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being (1st ed.). National Academies Press.
- Chang, B. P., & Cato, K. (2020, September). Tackling Burnout With Team Science: Nursing and Physician Collaborations on Improving Psychological Well-Being Among Emergency Clinicians. Journal of Emergency Nursing, 46(5), 557–559. https://doi.org/10.1016/j.jen.2020.05.009